Insulin resistance is a term that appears frequently in conversations about blood sugar, weight management, metabolic health, and long-term wellbeing. Despite how often it is mentioned, many people are unclear about what insulin resistance actually means, why it develops, and how everyday habits can influence it.
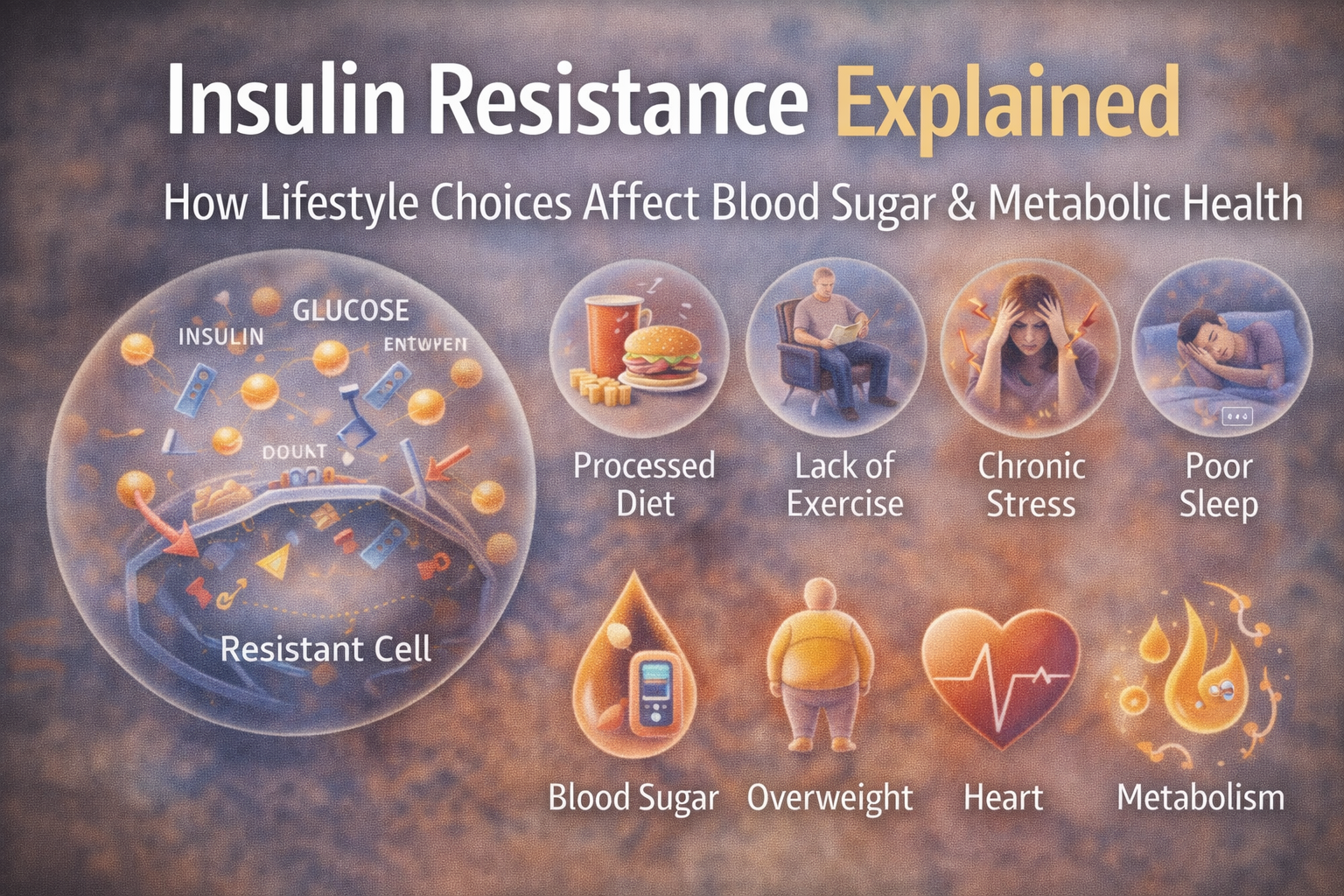
In the UK and globally, insulin resistance has become increasingly common, largely due to modern lifestyle patterns. Sedentary routines, highly processed diets, irregular sleep, and chronic stress all interact with how the body manages energy. While insulin resistance is often discussed alongside conditions such as type 2 diabetes, it is best understood as a metabolic state that can exist long before any diagnosis is made.
This in-depth guide explains insulin resistance in clear, practical terms. It explores how insulin works in the body, what happens when cells become resistant, which lifestyle factors influence insulin sensitivity, and how sustainable habits may support metabolic balance over time. The focus is educational, AdSense-safe, and designed to help readers make informed choices without fear or misinformation.
What Insulin Is And Why The Body Needs It
Insulin is a hormone produced by the pancreas. Its primary role is to help regulate blood sugar levels by allowing glucose to move from the bloodstream into cells, where it can be used for energy.
Insulin As An Energy Regulator
When you eat foods that contain carbohydrates, they are broken down into glucose. This glucose enters the bloodstream, causing blood sugar levels to rise. In response, the pancreas releases insulin, which signals cells to absorb glucose for immediate energy or storage.
Without insulin, glucose would remain in the bloodstream, and cells would struggle to access the energy they need to function properly.
Insulin Works Throughout The Day
Insulin is not only released after large meals. It plays a role throughout the day in maintaining stable blood sugar levels, supporting energy balance, and regulating how nutrients are stored and used.
Understanding Insulin Resistance In Simple Terms
Insulin resistance occurs when cells become less responsive to insulin’s signals. As a result, glucose has a harder time entering cells, leading to higher levels of sugar circulating in the bloodstream.
What “Resistance” Really Means
Insulin resistance does not mean insulin stops working entirely. Instead, it means cells require more insulin than usual to respond effectively. To compensate, the pancreas may produce more insulin in an attempt to keep blood sugar levels stable.
Over time, this increased demand can place strain on the body’s regulatory systems.
Insulin Resistance Exists On A Spectrum
Insulin resistance is not an on-or-off condition. It develops gradually and can exist for years without obvious symptoms. Early stages may be subtle, making awareness and prevention particularly important.
Why Insulin Resistance Matters For Health
Insulin resistance affects how efficiently the body uses energy. When glucose remains in the bloodstream rather than entering cells, multiple systems can be affected.
Blood Sugar Balance And Energy Levels
People with insulin resistance may experience:
- Energy highs followed by crashes
- Feeling tired after meals
- Increased hunger shortly after eating
These experiences are influenced by many factors, but insulin sensitivity plays a role in how steady energy levels feel throughout the day.
Long-Term Metabolic Impact
Persistently elevated blood sugar and insulin levels may contribute to broader metabolic challenges over time. This is why insulin resistance is often discussed in relation to long-term health monitoring.
Common Lifestyle Factors That Contribute To Insulin Resistance
Insulin resistance is influenced by a combination of genetic predisposition and lifestyle habits. While genetics cannot be changed, many lifestyle factors are modifiable.
Nutrition And Insulin Sensitivity
Diet plays a central role in how the body manages blood sugar and insulin.
Highly Processed Foods And Blood Sugar Spikes
Foods high in refined carbohydrates and added sugars are quickly digested, leading to rapid increases in blood sugar. Frequent spikes may increase insulin demand over time.
Examples include:
- Sugary drinks
- White bread and pastries
- Confectionery
- Highly processed snacks
The Importance Of Balanced Meals
Meals that combine carbohydrates with protein, healthy fats, and fibre tend to produce slower, steadier rises in blood sugar.
Balanced meals may include:
- Whole grains with vegetables and protein
- Legumes paired with healthy fats
- Fruits combined with yoghurt or nuts
Fibre And Blood Sugar Regulation
Fibre slows digestion and glucose absorption. Fibre-rich foods such as vegetables, oats, beans, lentils, and whole grains support steadier blood sugar responses.
Physical Activity And Insulin Sensitivity
Movement is one of the most effective ways to support insulin sensitivity.
How Exercise Helps Cells Use Glucose
Physical activity encourages muscles to absorb glucose independently of insulin. This means glucose can enter cells more easily during and after movement.
Types Of Activity That Support Insulin Sensitivity
- Walking and daily movement
- Resistance training
- Cycling or swimming
- Low-impact cardio
Consistency matters more than intensity. Regular moderate movement is often more sustainable than infrequent intense workouts.
Sedentary Behaviour And Metabolic Health
Prolonged sitting may reduce insulin sensitivity. Breaking up long periods of inactivity with short movement breaks can be beneficial.
Body Weight And Fat Distribution
Body weight and fat distribution influence insulin sensitivity, particularly fat stored around the abdomen.
Why Central Fat Matters
Abdominal fat is metabolically active and may influence insulin signalling. Reducing excess central fat through gradual lifestyle changes may support metabolic balance.
Focus On Health Not Rapid Weight Loss
Rapid or extreme weight loss approaches are often difficult to maintain and may disrupt metabolic health. Sustainable changes are more effective long term.
The Role Of Sleep In Insulin Resistance
Sleep plays a critical role in metabolic regulation.
How Poor Sleep Affects Blood Sugar
Lack of sleep may influence hormones that regulate appetite and insulin sensitivity. Even short-term sleep deprivation can affect how the body processes glucose.
Supporting Better Sleep Habits
- Consistent sleep schedules
- Reducing screen use before bed
- Creating a calm sleep environment
Quality sleep supports overall metabolic health.
Stress And Its Impact On Insulin Sensitivity
Stress triggers hormonal responses that influence blood sugar regulation.
Cortisol And Blood Sugar
Stress hormones encourage glucose release into the bloodstream to provide quick energy. Chronic stress may contribute to elevated blood sugar and increased insulin demand.
Managing Stress As Part Of Metabolic Health
Stress management strategies include:
- Gentle movement
- Mindfulness or breathing exercises
- Time outdoors
- Regular rest and breaks
Gut Health And Insulin Resistance
The digestive system and gut microbiome play a role in metabolic health.
Gut Bacteria And Blood Sugar Regulation
Gut microorganisms influence inflammation, nutrient absorption, and hormone signalling. A balanced gut environment supports overall metabolic function.
Supporting Gut Health Naturally
- Eating fibre-rich foods
- Including fermented foods where appropriate
- Managing stress and sleep
Early Signs Often Associated With Insulin Resistance
Insulin resistance can develop silently, but some people notice subtle changes.
Commonly Reported Experiences
- Increased fatigue
- Difficulty managing weight
- Cravings for sugary or refined foods
- Feeling hungry soon after meals
These experiences are not diagnostic but may indicate the need for lifestyle reflection or professional guidance.
Insulin Resistance And Long-Term Health Monitoring
Insulin resistance is often identified through blood tests and clinical assessment.
Understanding Blood Test Results
Healthcare professionals may look at:
- Fasting blood glucose
- Long-term blood sugar markers
- Insulin levels
- Overall metabolic profile
Results are best interpreted in context rather than in isolation.
Common Myths About Insulin Resistance
Myth One Only Overweight People Develop Insulin Resistance
Insulin resistance can occur in people of various body sizes due to genetics, stress, inactivity, or sleep disruption.
Myth Two Carbohydrates Must Be Eliminated
Carbohydrates can be part of a balanced diet. Quality, portion size, and food combinations matter more than complete avoidance.
Myth Three Insulin Resistance Happens Overnight
Insulin resistance develops gradually and is influenced by long-term patterns.
Supporting Insulin Sensitivity Through Sustainable Habits
Improving insulin sensitivity is not about extreme changes but consistent habits that support metabolic balance.
Practical Daily Strategies
- Eat regular, balanced meals
- Include movement most days
- Prioritise sleep
- Manage stress
- Reduce prolonged sitting
Small changes practised consistently can have meaningful effects over time.
When To Seek Professional Advice
Anyone concerned about blood sugar, metabolic health, or insulin resistance should consult a qualified healthcare professional.
Situations Where Guidance May Be Helpful
- Family history of metabolic conditions
- Persistent fatigue or energy crashes
- Difficulty managing weight despite lifestyle changes
- Abnormal blood test results
Professional assessment ensures advice is tailored and appropriate.
A Balanced Perspective On Insulin Resistance
Insulin resistance is not a personal failure. It reflects how modern lifestyles interact with human biology. Understanding insulin resistance empowers individuals to make informed, realistic changes that support long-term health.
By focusing on balanced nutrition, regular movement, quality sleep, stress management, and gut health, many people can support insulin sensitivity naturally and sustainably.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. It is not intended to diagnose, treat, cure, or prevent any medical condition. Always consult a qualified healthcare professional regarding concerns about blood sugar, insulin resistance, or metabolic health.